Getting Better Results for GI Cancer Patients
Mark Yarchoan, M.D.
Mark Yarchoan, M.D., is actively pursing several ways to make immunotherapy work better for patients with gastrointestinal cancers, including pancreatic, colon, liver and bile duct cancers.
“Immunotherapy has not worked as well in GI cancers as some other cancers, and we want to study new ways to make them more sensitive to immunotherapy treatments,” says Yarchoan.
Yarchoan and colleagues are exploring several approaches, including the use of vaccines to attract the immune system to the tumor. The vaccine is combined with a checkpoint inhibitor to prevent the immune cells that are stimulated by the vaccine from shutting down once they reach the tumor. An added aspect to this research is the development of new types of vaccines that may do a better job of rousing an immune response.
“There are two parts to vaccines. One part tells immune cells what to attack, and the other stimulates the immune system,” says Yarchoan. “Most cancer treatment vaccines have used GMCSF, a protein secreted by immune cells, to incite an immune response. We are trying to develop a new kind of adjuvant that works quite differently to maximally stimulate the immune system.”
He and Skip Viragh Center Co-Director, Daniel Laheru, M.D., are collaborating on a study that uses a pancreatic cancer vaccine and the anti-PD-1 drug nivolumab before surgery to see if it can generate an immune response to shrink tumors and make them more amenable to surgical removal and less likely to recur. This study is funded by Fran and Jim McGlothlin.
Yarchoan is collaborating with Precision Medicine Center of Excellence Co-Director Lei Zheng, M.D., Ph.D., and colon cancer expert Nilo Azad, M.D., on a novel approach to make colon cancer more responsive to immunotherapy. The work builds upon an earlier discovery by Skip Viragh Center clinician-scientist Dung Le, M.D., that linked a cancer cell defect known as microsatellite instability to response to the immunotherapy drug pembrolizumab. They are exploring whether a cancer vaccine that stimulates the immune system can convert microsatellite-stable colon cancers that are currently not responsive to pembrolizumab to immunotherapy responders.
In bile duct cancer, he and Azad are leading a national clinical trial through the National Cancer Institute’s Cancer Therapy Evaluation Program to study the combination of the MEK inhibitor cobimetinib with the PD-L1 immune checkpoint inhibitor atezolizumab. It is the first clinical trial for bile duct cancer patients whose cancers come back following chemotherapy.
“We want to see if cobimetinib combined with atezolizumab works better than atezolizumab alone,” says Yarchoan. “There is currently no effective treatment for patients who progress after chemotherapy, and survival for these patients is unfortunately often measured in months,” says Yarchoan.
In liver cancer, he has started the first clinical trial of an immune checkpoint inhibitor before surgery. The trial uses an immune checkpoint inhibitor plus another drug called cabozantinib to try to shrink liver cancers before surgery and hopefully improve the chances of a successful and curative surgery. Yarchoan believes that cabozantinib may change the tumor to be more responsive to the immune checkpoint inhibitor while also helping to eliminate micrometastases, microscopic cells that can seed the spread of cancer.
“We hope this will improve the chance of cure,” says Yarchoan, who is collaborating with Laheru to also see if cabozantinib alters the cellular environment of tumors to improve the activity of nivolumab.
Targeted Vaccines
Neeha Zaidi, M.D.
Certain antigens can help the immune system distinguish cancer cells from normal cells. Neoantigens are proteins or signals from mutated cancer genes within a tumor that are unique to each patient’s cancer and, with a little help, can be recognized by the immune system.
Neeha Zaidi, M.D., is working on neoantigen-targeted vaccines for pancreatic and colon cancers. Using a pancreatic cancer model, she and her collaborators have identified the most immunogenic neoantigens—the ones that attract the greatest numbers of cancer-attacking immune T cells to the tumor. The current version of the vaccine includes 12 neoantigens, but Zaidi says additional ones could be added.
A clinical trial that combines neoantigen-targeted vaccines with two other immunotherapy drugs, known as checkpoint inhibitors, is planned. While the vaccine draws immune cells to the tumor, the drugs release important brakes on the immune response. One drug will target and block PD-1, an immune “stop” signal exploited by cancer cells, and the other interferes with an immune signal called OX40 to stimulate production of more immune T cells.
This approach builds on another Skip Viragh Center discovery, showing that cancers with a defect known as microsatellite instability accumulate large numbers of mutations that serve as red flags for the immune system. Cancers with MSI tend to draw the attention of the immune system and, with the addition of a checkpoint inhibitor, respond well to immunotherapy. Zaidi believes the vaccine/drug combination can make microsatellite-stable cancers look like MSI cancers and generate an immune response to the cancer.
“Our goal is to make more cancers respond to immunotherapy by making their mutations visible to the immune system,” says Zaidi.
Clinical Trials for Treatment-Resistant Cancers
 Katherine Bever, M.D. and patient Sandra Myers
Katherine Bever, M.D. and patient Sandra MyersKatherine Bever, M.D., is collaborating with Dung Le, M.D., on a clinical trial for patients with advanced pancreatic cancers that have spread outside of the pancreas. The trial combines a the pancreatic cancer vaccine to bring cancer-killing T cells to pancreatic tumors with drugs that block two immune checkpoints, called PD-1 and IDO, that cancer cells hijack to shut down the immune response. The combination therapy is followed by a listeria vaccine engineered to express mesothelin, an immune cell-alerting signal common to pancreatic cancer. The trial is designed for patients who did not respond to the pancreatic cancer vaccine and anti-PD-1 immunotherapy. Bever hopes the four-pronged approach will work synergistically to stimulate the immune system while also removing cancer-imposed brakes on the immune response.
With funding from Swim Across America, Bever has also begun research of high-grade neuroendocrine tumors, a very aggressive type of pancreatic cancer that often responds poorly to treatment. She will be exploring the microenvironment, the cellular environment in which the tumor lives, for clues that could lead to ways to make these tumors respond to immunotherapy with checkpoint inhibitors.
Extending Progress to Other Cancers

Evanthia Torress, M.D., Ph.D.

Roisin Connolly, M.B.B.Ch.
Evanthia Roussos Torres, M.D., Ph.D., is taking what she learned working in the lab of Elizabeth Jaffee, M.D., to help patients with breast cancer, but the precision medicine model she is developing for HER2-positive breast cancer can also be applied to pancreatic cancer.
The research is aimed at converting nonimmunogenic tumors—ones that don’t respond to immunotherapy—to immunogenic tumors—ones that respond well to immunotherapy.
HER2-positive breast cancer produces a cancer cell growth-stimulating protein known as the human epidermal growth factor receptor 2. Therapies that target HER2, like the drug trastuzumab (Herceptin), have improved survival, but a significant number of breast cancer patients see their cancers return. Roussos Torres’ approach involves using a combination of the immune checkpoint inhibitors ipilimumab and nivolumab with an epigenetic-targeted drug called entinostat. Checkpoint inhibitors release important brakes the cancer cell puts on the immune response, and the epigenetic drug changes the chemical environment of cells to make them more amenable to immunotherapy.
“Basically, we believe this treatment combination allows immune T cells to infiltrate tumor cells and to do a better job,” says Roussos Torres.
Engaging the immune system to fight cancer has been shown to prevent cancers from coming back, resulting in long-lasting responses in several tumor types. In the laboratory, Roussos
Immunotherapy works extraordinarily well in a subset of cancer patients—sometimes making what were thought to be incurable cancers curable. However, it doesn’t work in all patients. Tara Robinson, M.D., Ph.D., is focused on understanding why this promising new cancer treatment works so well in some patients and not in others. What she learns may lead to precision medicine approaches that make immunotherapy more effective and an option for more patients.
Robinson says a lot of effort has been placed on understanding the tumor, including the genetic changes that drive growth and drugs that can target these genetic changes. For her research, she has chosen a different path, looking instead at what cancer cells, and the treatments we use to combat them, do to the immune system.
“I want to know how cancer and cancer therapy change the immune system to find new opportunities to improve treatment responses,” she says.
A breast cancer study from the 1990s that showed chemotherapy had a long-lasting impact on immune cells, with T cells and B cells taking up to two years to return to normal function, led her to explore the effect of chemotherapy on each type of immune cell.
“Immunotherapy has become a first-line treatment for some cancers, but in general, we use it when a patient’s cancer does not respond to traditional chemotherapy,” says Robinson. She wonders if previous treatment with chemotherapy could be dampening the immune response in some patients.
“When we talk about immunotherapy, we compare the immune system to a car and use an analogy of releasing the brakes to get the car, aka the immune system, moving, but what if your car is totaled? Releasing the brakes really won’t be much help,” she says.
The science of immunology, and technologies available to researchers, has improved dramatically since that 1990s breast cancer study was published, and Robinson is using a mouse model of pancreatic cancer to precisely measure the effect of chemotherapy on subsets of immune cells, including cells that suppress immune activity.
“When a tumor is established and growing and the patient gets chemotherapy, how does that change the game? This is an area that is underinvestigated,” she says. “Even with the predicted growth in immunotherapy, most cancer patients will still receive chemotherapy at some point. We need to know what it’s doing to the immune system.”
Ultimately, she hopes to use her findings to help guide immunotherapy based on the type of chemotherapy patients have received.
“The impact on immune cells may be different for patients who have never had chemotherapy or have received one type of chemotherapy versus another. Different chemotherapy drugs may have varying affects on immune cells. Understanding these differences can tell us what types of immunotherapy are likely to work in a patient and what approaches may not work,” says Robinson. “This is personalized treatment based on immune parameters rather than tumor parameters.”
has zeroed in on about a half-dozen genes that can be epigenetically targeted to decrease immune suppression. Although etinostat broadly hits many genes, she is working to tease out certain genes to develop a precision approach that more specifically hits genes that are only specific to improving the response to anticancer therapies.
“We think there may be interplay between the trastuzumab (Herceptin) signaling pathway and immune checkpoint inhibition occurring through etinostat,” she says. “ We need to flesh that out so we can understand how these signaling pathways are talking to one another to get the desired response.”
She is collaborating with breast cancer expert Roisin Connolly, M.B.B.Ch., to evaluate the combination therapy in patients.
“In a clinical trial, we will be able to isolate responders from nonresponders and compare what we see to laboratory models to better understand the mechanisms,” says Roussos Torres. This will allow them to identify biomarkers that will help guide the therapy to those patients most likely to benefit.
Cancer Versus the Immune System
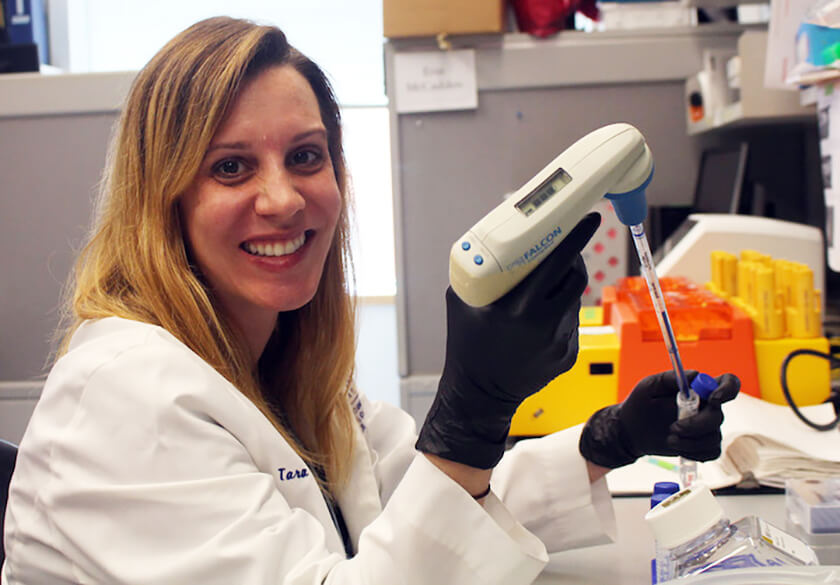
Tara Robinson, M.D., Ph.D.
Immunotherapy works extraordinarily well in a subset of cancer patients—sometimes making what were thought to be incurable cancers curable. However, it doesn’t work in all patients. Tara Robinson, M.D., Ph.D., is focused on understanding why this promising new cancer treatment works so well in some patients and not in others. What she learns may lead to precision medicine approaches that make immunotherapy more effective and an option for more patients.
Robinson says a lot of effort has been placed on understanding the tumor, including the genetic changes that drive growth and drugs that can target these genetic changes. For her research, she has chosen a different path, looking instead at what cancer cells, and the treatments we use to combat them, do to the immune system.
“I want to know how cancer and cancer therapy change the immune system to find new opportunities to improve treatment responses,” she says.
A breast cancer study from the 1990s that showed chemotherapy had a long-lasting impact on immune cells, with T cells and B cells taking up to two years to return to normal function, led her to explore the effect of chemotherapy on each type of immune cell.
“Immunotherapy has become a first-line treatment for some cancers, but in general, we use it when a patient’s cancer does not respond to traditional chemotherapy,” says Robinson. She wonders if previous treatment with chemotherapy could be dampening the immune response in some patients.
“When we talk about immunotherapy, we compare the immune system to a car and use an analogy of releasing the brakes to get the car, aka the immune system, moving, but what if your car is totaled? Releasing the brakes really won’t be much help,” she says.
The science of immunology, and technologies available to researchers, has improved dramatically since that 1990s breast cancer study was published, and Robinson is using a mouse model of pancreatic cancer to precisely measure the effect of chemotherapy on subsets of immune cells, including cells that suppress immune activity.
“When a tumor is established and growing and the patient gets chemotherapy, how does that change the game? This is an area that is underinvestigated,” she says. “Even with the predicted growth in immunotherapy, most cancer patients will still receive chemotherapy at some point. We need to know what it’s doing to the immune system.”
Ultimately, she hopes to use her findings to help guide immunotherapy based on the type of chemotherapy patients have received.
“The impact on immune cells may be different for patients who have never had chemotherapy or have received one type of chemotherapy versus another. Different chemotherapy drugs may have varying affects on immune cells. Understanding these differences can tell us what types of immunotherapy are likely to work in a patient and what approaches may not work,” says Robinson. “This is personalized treatment based on immune parameters rather than tumor parameters.”
Finding the Right Combination

May Tun Saung, M.D.
May Tun Saung, M.D., is conducting several clinical studies building upon laboratory research that showed adding a macrophage-modifying drug to a pancreatic cancer vaccine and anti-PD1 checkpoint inhibitor combination may improve the immune response to pancreatic cancer.
Macrophages are a type of white blood cell that play a critical role in the body’s immune response but are corrupted by cancer cells to help the tumor instead of destroying it.
Saung’s approach uses the vaccine to draw cancer-killing immune cells to the tumor and an anti-PD1 checkpoint inhibitor and a macrophage-targeted drug to convert immune suppressing signals to immune-activating signals.
In pancreatic cancer animal models, immune T cell activation went up and survival was extended when the macrophage-targeted drug was added to the vaccine and anti-PD1 drug combination. Saung is working to translate these laboratory findings to patients. Although immune markers indicate similar activity in patients, the triple combination has not worked much better than the anti-PD1/vaccine combo in patients.
“It looks like T cells do better when we add the macrophage-stimulating drug,” says Saung. “That’s the expression end of the things. Now we have to go back to the laboratory and look at function.”
